2021
Download Handbook volume 1 (49MB)
Download Handbook volume 2 (55MB)
2020
The second summer school of
the BrainIT project (initially scheduled for July 2020, but delayed due
to the pandemic situation) focused on neuro-oncology. For the practical
sessions, two real cases of brain tumor have been developed:
·
Meningioma case, which is a brain tumor arising from the meninges
(the membranous layers surrounding the brain). The consistency of the tumor is
higher than the one of the brain.
·
Glioma case, which is a brain tumor located in any area of the
brain and with lower consistency than the brain (removable by vacuum).
As in the previous section, both
cases had to be developed starting from the DICOM images of the patients and
with low-cost manufacturing approaches (material extrusion AM). Ten replicas of
each case had to be obtained for the practical training sessions. In both
cases, the students will cut the skull and access the tumor to be removed with
hand tools (meningioma) or by vacuum (glioma). Finally, the removed bone will
be sutured again.
Case 1: Meningioma.
This type of tumor has a higher
consistency than brain. For this reason, a stiffer blend compared to the brain
was used to produce the tumor (1:1 rate of components A:B of Ecoflex 00-10). Furthermore,
considering that this tumor is reddish in color and contains calcium deposits,
it was decided to add a small amount of a red pigment (3% of the total mass),
in addition to crushed PLA that simulates calcification, thus achieving a more
realistic model.
Case 2: Glioma
This
tumor has a lower consistency than brain. For this reason and with the
experience obtained with the material chosen to emulate the hematoma of case 1
of the first summer school (Figure
24),it was decided to simulate this model with
a mixture of sodium alginate with distilled water in a ratio of 1:20 w/w.
The process started with the
segmentation of the real CT images (DICOM files). In this case, the models to
be segmented will be the same as in the previous case, except the tumor, which
will not be poured in a mold, but inside the molded brain. Therefore, a cavity
must be defined inside the molded brain to pour the sodium alginate solution
that mimics the tumor.
Training material for
neurovascular surgery
The third summer school of the BrainIT project focused on
neurovascular surgery. For this summer school, synthetic models of an aneurysm
located in the medial cerebral artery (MCA aneurysm) were
developed. As this document is being written before this summer school (August
2021), the current section shows all the design process and tests carried out
so far, without having finished the complete manufacturing process.
Synthetic models ofa medial cerebral artery aneurysm was developed, starting from the
real case depicted in Figure 101.
Figure 101. CT images of a real
case of MCA aneurysm.
For the manufacture of blood
vessels,the Digital Anatomy Printer (DAP) technology was selected, as it has a
wide range of materials to mimic anatomy tissues. In order to choose the best
material option and thickness of the vessels, 9 tube-shaped samples were
manufactured and tested by neurosurgeons to find the best option to mimic real
brain blood vessels for the surgery training.
2019
The first summer school of
the BrainIT project (July 2019) focused on trauma in neurosurgery. Two
cases were developed for the practical sessions of this summer school:
·
An intracranial hematoma with large skull fracture
·
An intracranial hematoma, without skull fracture
Both cases were developed
starting from the real scanning images of the patients and with low-cost
manufacturing approaches. Material extrusion AM was used to produce 10 replicas
of each case for the practical training sessions. In both cases, the students
had to cut the skull in the correct area, remove the hematoma by vacuum and
place/sew again the removed bone.
Regarding the hematoma material,
after different tests with different concentrations, the final choice was a
solution of sodium alginate powder (from Acros Organics) with distilled water
(1:20 w/w). This solution was also approved by the surgeon to simulate the
hematoma.
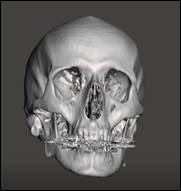
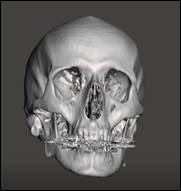
The first case was an
intracranial hematoma with skull fracture (the patient suffered a severe trauma
with a large fracture).
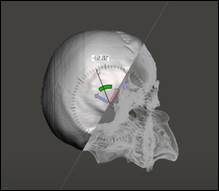
Once selected the material for
the skull and hematoma, the 3D reconstruction was made by using the CT scan
images of the patient and processing them in the 3D Slicer software
(segmentation process).
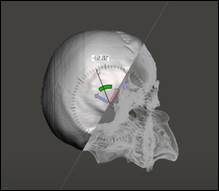
In order to reduce the cost and facilitate the fixation of
the skulls for the practical training sessions, the skull was cut in the
Meshmixer software to focus on the region of interest, thus removing the lower
part of the model




The second case consisted in another intracranial hematoma,
but in this case the skull did not have any fracture. The process was similar
to the previous one and the same materials were used.
The process started with the segmentation of the real CT
images (DICOM files). In this case, during the segmentation of the skull, a
wall that surrounds the hematoma was also segmented to obtain the cavity of the
hematoma.

This figure shows the skull during the practical training of
students (after the cutting of bone, removal of the hematoma and suture of the
removed bone). Note that the sodium alginate solution to emulate the hematoma
was also filled in situ before the practical session (the hole of the
base was sealed with the cylindrical and flexible 3D printed caps, as in case
1).
2020
The second summer school of the BrainIT project (initially scheduled for July 2020, but delayed due to the pandemic situation) focused on neuro-oncology. For the practical sessions, two real cases of brain tumor have been developed:
· Meningioma case, which is a brain tumor arising from the meninges (the membranous layers surrounding the brain). The consistency of the tumor is higher than the one of the brain.
· Glioma case, which is a brain tumor located in any area of the brain and with lower consistency than the brain (removable by vacuum).
As in the previous section, both cases had to be developed starting from the DICOM images of the patients and with low-cost manufacturing approaches (material extrusion AM). Ten replicas of each case had to be obtained for the practical training sessions. In both cases, the students will cut the skull and access the tumor to be removed with hand tools (meningioma) or by vacuum (glioma). Finally, the removed bone will be sutured again.
Case 1: Meningioma.
This type of tumor has a higher consistency than brain. For this reason, a stiffer blend compared to the brain was used to produce the tumor (1:1 rate of components A:B of Ecoflex 00-10). Furthermore, considering that this tumor is reddish in color and contains calcium deposits, it was decided to add a small amount of a red pigment (3% of the total mass), in addition to crushed PLA that simulates calcification, thus achieving a more realistic model.
Case 2: Glioma
This tumor has a lower consistency than brain. For this reason and with the experience obtained with the material chosen to emulate the hematoma of case 1 of the first summer school (Figure 24),it was decided to simulate this model with a mixture of sodium alginate with distilled water in a ratio of 1:20 w/w.
The process started with the segmentation of the real CT images (DICOM files). In this case, the models to be segmented will be the same as in the previous case, except the tumor, which will not be poured in a mold, but inside the molded brain. Therefore, a cavity must be defined inside the molded brain to pour the sodium alginate solution that mimics the tumor.
Training material for neurovascular surgery
The third summer school of the BrainIT project focused on neurovascular surgery. For this summer school, synthetic models of an aneurysm located in the medial cerebral artery (MCA aneurysm) were developed. As this document is being written before this summer school (August 2021), the current section shows all the design process and tests carried out so far, without having finished the complete manufacturing process.
Synthetic models ofa medial cerebral artery aneurysm was developed, starting from the real case depicted in Figure 101.
Figure 101. CT images of a real case of MCA aneurysm.
For the manufacture of blood vessels,the Digital Anatomy Printer (DAP) technology was selected, as it has a wide range of materials to mimic anatomy tissues. In order to choose the best material option and thickness of the vessels, 9 tube-shaped samples were manufactured and tested by neurosurgeons to find the best option to mimic real brain blood vessels for the surgery training.
2019
The first summer school of the BrainIT project (July 2019) focused on trauma in neurosurgery. Two cases were developed for the practical sessions of this summer school:
· An intracranial hematoma with large skull fracture
· An intracranial hematoma, without skull fracture
Both cases were developed starting from the real scanning images of the patients and with low-cost manufacturing approaches. Material extrusion AM was used to produce 10 replicas of each case for the practical training sessions. In both cases, the students had to cut the skull in the correct area, remove the hematoma by vacuum and place/sew again the removed bone.
Regarding the hematoma material, after different tests with different concentrations, the final choice was a solution of sodium alginate powder (from Acros Organics) with distilled water (1:20 w/w). This solution was also approved by the surgeon to simulate the hematoma.
The first case was an intracranial hematoma with skull fracture (the patient suffered a severe trauma with a large fracture).
Once selected the material for the skull and hematoma, the 3D reconstruction was made by using the CT scan images of the patient and processing them in the 3D Slicer software (segmentation process).
In order to reduce the cost and facilitate the fixation of the skulls for the practical training sessions, the skull was cut in the Meshmixer software to focus on the region of interest, thus removing the lower part of the model




The second case consisted in another intracranial hematoma, but in this case the skull did not have any fracture. The process was similar to the previous one and the same materials were used.
The process started with the segmentation of the real CT images (DICOM files). In this case, during the segmentation of the skull, a wall that surrounds the hematoma was also segmented to obtain the cavity of the hematoma.

This figure shows the skull during the practical training of students (after the cutting of bone, removal of the hematoma and suture of the removed bone). Note that the sodium alginate solution to emulate the hematoma was also filled in situ before the practical session (the hole of the base was sealed with the cylindrical and flexible 3D printed caps, as in case 1).